Feb 3, 2026
by Nikhil Pai
A medical chronology is a structured timeline that organizes a claimant's medical history by date, linking diagnoses, treatments, and functional limitations to specific time periods. Creating one involves seven steps: gathering records from all treating sources, sorting by provider and date, extracting key data points, building the timeline, summarizing functional limitations, cross-referencing with RFC and Listing criteria, and conducting a final quality review. The process transforms disorganized medical records into a document that supports hearing preparation and brief writing.
Medical records arrive in stacks. Sometimes digital, sometimes paper, often both. They come from hospitals, specialists, primary care offices, therapists, and pharmacies. Each source uses its own format, its own date conventions, its own abbreviations. Somewhere in that pile is the evidence that determines whether your client gets approved at their ALJ hearing.
A medical chronology transforms that pile into something an Administrative Law Judge can actually use. It maps a claimant's treatment history against their functional limitations, and it creates a timeline that tells the story of their disability. When done well, the chronology becomes the backbone of hearing preparation. When done poorly, or rushed, or skipped, it creates gaps that ALJs notice and question.
What follows is the medical chronology process step by step. The goal is a repeatable process your team can use on every case, regardless of who handles the file.
What Is a Medical Chronology?
Most attorneys have encountered medical summaries before. A summary captures high-level facts: diagnoses, treating physicians, current medications. A chronology does something different.
A medical chronology is a structured timeline that organizes a claimant's medical history in date order, linking diagnoses, treatments, and provider notes to specific periods of time. It tracks when conditions were first documented, how treatment progressed, what functional limitations were noted over time, and where gaps exist in the record. It is a reference document for hearing preparation and brief writing, though its value depends on how thoroughly the underlying records were gathered.
For disability hearings, the chronology serves three purposes:
Evidence organization: A single document that maps all medical evidence to dates, which makes locating specific records during hearing prep considerably easier.
Narrative construction: The foundation for building the story of disability progression that ALJs need to evaluate severity and duration.
Gap identification: A mechanism for surfacing missing records or treatment interruptions before they become problems at the hearing.
ALJs evaluate disability claims under SSA's five-step sequential evaluation. Medical evidence is central to Steps 2 through 5. A well-constructed chronology makes it easier to demonstrate that a claimant's condition meets severity and duration requirements, and to support RFC assessments with specific clinical documentation. The chronology itself is an organizational tool, not a substitute for strong underlying evidence.
Why Medical Chronologies Matter for Disability Hearings
SSA uses a five-step sequential evaluation to determine whether a claimant is disabled. At Step 2, the claimant must show a severe medically determinable impairment. At Step 3, SSA assesses whether the impairment meets or equals a Listing. Steps 4 and 5 evaluate residual functional capacity and ability to work.
Medical evidence drives each of these determinations.
Picture an ALJ reviewing a 1,500-page medical file without a chronology. They have to piece together the treatment timeline themselves. They may miss a functional capacity note buried in a progress report from two years ago. They may not notice that treatment gaps coincide with insurance lapses rather than symptom improvement. They draw conclusions from incomplete context.
A chronology does the organizational work in advance. It puts the evidence in sequence, highlights functional limitations at each stage, and makes it easier for the ALJ to follow the disability narrative.
Chronologies matter most for cases that do not meet a Listing outright. When you are arguing RFC limitations at Steps 4 and 5, the timeline of functional decline and treatment response becomes central. A chronology that maps functional capacity notes across the treatment period supports those arguments more effectively than disorganized records.
Step-by-Step Process for Creating a Medical Chronology
The following process produces a consistent, usable chronology regardless of case complexity. Timing and depth can be adapted based on record volume, but the sequence should remain the same.
Step 1: Gather All Medical Records from Treating Sources
Start with a complete provider list. Pull records from primary care, specialists, hospitals, urgent care, mental health providers, and physical therapists. Request pharmacy records for medication history. Include imaging reports and lab results.
Do not assume the records SSA has on file are complete. Request directly from providers when possible, and note any sources that have not responded. You will need to follow up or document the gap. In some cases the missing records turn out to be the most important ones in the file. This pattern becomes apparent only in retrospect, which argues for aggressive early outreach even when a case seems straightforward.
Step 2: Sort Records by Provider and Date
Organize records first by provider, then chronologically within each provider's set. This makes it easier to track treatment continuity with each source before combining into a unified timeline.
Use consistent date formatting throughout. If providers use different formats (MM/DD/YYYY vs. DD/MM/YYYY), standardize before proceeding.
Step 3: Extract Key Data Points
For each record, extract:
Date of service
Provider name and specialty
Diagnoses documented
Treatments provided or prescribed
Functional limitations noted (mobility restrictions, cognitive issues, fatigue levels, pain assessments)
Medications (new prescriptions, dosage changes, discontinuations)
Referrals or follow-up instructions
Functional capacity notes deserve particular attention. These often appear in progress notes rather than formal assessments. A sentence like "patient reports difficulty standing for more than 10 minutes" is RFC evidence, even if it does not appear in a dedicated functional capacity form.
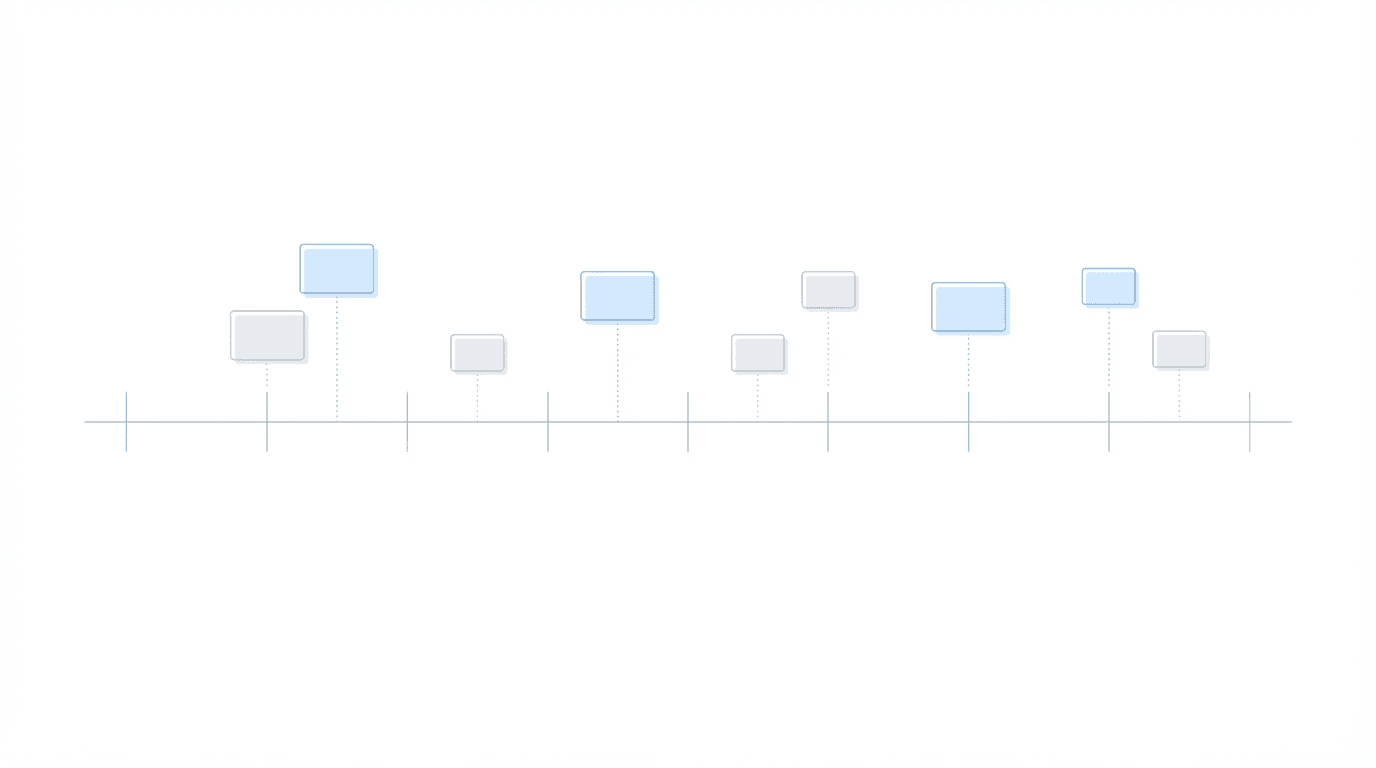
Step 4: Build the Timeline
Combine extracted data into a single chronological timeline. Each entry should include the date, provider, and key findings from that visit.
Flag gaps. If a claimant saw their cardiologist every three months for a year, then has no cardiology records for eight months, note that. You may need to obtain missing records. You may need to prepare to explain the gap at hearing. Sometimes the explanation matters more than the gap itself.
Mark significant events: hospitalizations, surgeries, new diagnoses, medication changes, documented worsening.
Step 5: Summarize Functional Limitations and Treatment Compliance
Add a functional limitations summary that tracks how capacity changed over time. Note when limitations were first documented, whether they worsened or stabilized, and what clinical evidence supports each limitation.
Document treatment compliance. SSA evaluates whether claimants follow prescribed treatment. If the chronology shows consistent follow-up and medication adherence, note that. If there are gaps, identify whether they correlate with insurance issues, provider availability, or other explanatory factors.
Step 6: Cross-Reference with RFC and Listing Criteria
Review the chronology against the relevant Listing of Impairments. Note entries that document clinical criteria from the Listings. For RFC arguments, identify specific chronology entries that support each functional limitation. When writing the pre-hearing brief, reference these directly.
Step 7: Review and Quality Check
Before finalizing, check for:
Missing dates or providers
Duplicate entries
Inconsistent terminology
Unsupported functional limitation claims
Gaps that need explanation
Have a second person review if possible. Fresh eyes catch things you've stopped seeing after hours in the same file.
Common Mistakes That Weaken Medical Chronologies
Missing records or incomplete provider lists: if you do not have records from a treating source, the chronology has a gap. ALJs notice when a claimant reports seeing a specialist but no records from that specialist appear in the file. Build a complete provider list at intake and track which sources have responded.
Inconsistent date formatting: mixed formats cause sequencing errors. A record dated 03/04/2023 could be March 4 or April 3 depending on the source's format.
Overlooking functional capacity notes in progress reports: formal RFC assessments are obvious evidence. But functional limitations are often documented in passing: "patient unable to lift groceries," "reports difficulty concentrating for more than 20 minutes," "observed limping during exam." These notes matter. Their cumulative weight often exceeds the impact of any single formal assessment.
Failing to flag treatment gaps: a six-month gap in treatment for a condition claimed as disabling raises questions. Did the condition improve? Did the claimant lose insurance? Did they move and lose access to their provider? If you do not flag the gap, you cannot prepare to address it.
Rushing chronology prep under deadline pressure: when exhibit deadlines approach and the chronology is not done, errors multiply. Building chronologies earlier in the case lifecycle prevents this, though the pressure to prioritize urgent matters over important ones is constant.
How Technology Helps Disability Firms Build Better Chronologies
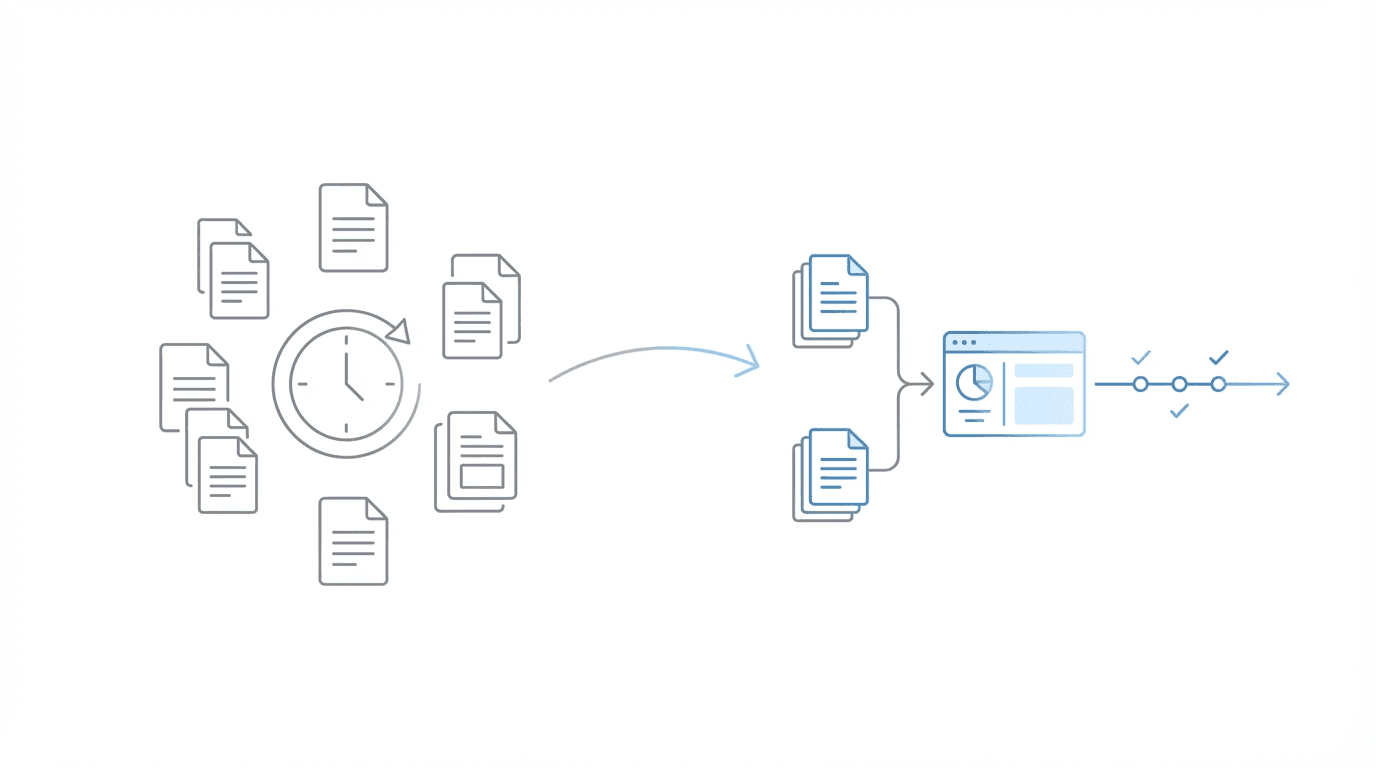
Manual chronology creation is labor-intensive. A complex case with 2,000 pages of medical records can take a paralegal multiple days to process. Multiply that across dozens or hundreds of active cases, and chronology work becomes a capacity constraint.
The challenge is not just time. Manual processes introduce inconsistency. Each paralegal develops their own extraction habits, their own formatting preferences, their own threshold for what counts as a significant finding. Chronologies vary in quality depending on who prepared them.
Technology addresses both problems. Chronology tools can extract structured data from medical records, apply consistent formatting, and surface functional limitation notes that manual review might miss. Output becomes more consistent. Staff time shifts from data extraction to quality review. Whether that shift produces better outcomes depends on how the firm uses the recovered time.
When evaluating chronology tools, consider whether they integrate with your case management workflow. A chronology that lives in a separate system creates handoff friction.
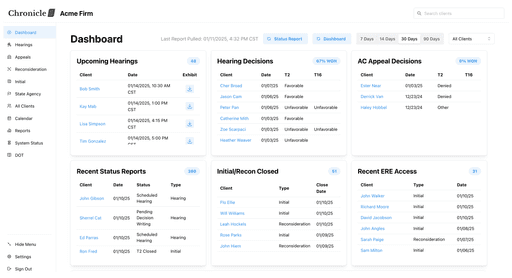
Chronicle supports medical chronology management as part of hearing preparation workflows. The approach integrates chronology output with case prep dashboards and deadline monitoring, so the work product connects to the broader hearing preparation process rather than sitting in isolation.
Firms using Chronicle have applied the medical chronology capabilities to large-file cases. At Anderson Marois & Associates, the team used Chronicle's medical chronology features for hearing preparation on a 2,000-page file. At Ficek Law, medical chronology work anchors hearing preparation. The workflow starts with a high-level summary from the chronology, then dives into specific records as needed. In that case study context, Tony Ficek reported a hearing approval rate of 70-75%, up from the low 60s.
Putting It Together: Medical Chronologies in Your Hearing Prep Workflow
The chronology is most useful when it connects to the rest of hearing preparation.
Build chronologies early enough to inform case strategy. Waiting until two weeks before the hearing means losing the ability to obtain missing records or develop additional evidence based on what the chronology reveals.
Use the chronology to structure pre-hearing briefs. When arguing functional limitations, reference specific chronology entries. When explaining treatment history, the chronology provides the narrative backbone.
Coordinate chronology completion with exhibit deadlines. SSA has specific deadlines for submitting evidence before hearings. A chronology finished after the exhibit deadline cannot include records you discover are missing.
Chronicle includes deadline monitoring and alerts to reduce missed tasks in case prep. Hearing preparation dashboards provide visibility into which cases have complete chronologies and which need attention before their deadlines.
Frequently Asked Questions
How long should a medical chronology be?
The question comes up often, and there is no fixed answer. A straightforward case with limited treatment history might produce a 5-10 page chronology. A complex case with multiple conditions and years of records might run 30-50 pages. Completeness matters more than page count.
Should I include every medical record in the chronology?
Not every visit belongs in the chronology. Include records relevant to the claimed disability and functional limitations. Routine visits unrelated to the disability (annual flu shots, unrelated acute care) can be noted briefly or omitted. The chronology should tell the disability story.
When should chronology prep start in the case lifecycle?
Most firms start too late. For cases heading toward hearing, begin chronology work at least 60-90 days before the exhibit deadline. This allows time to identify and obtain missing records.
Who should prepare medical chronologies?
Paralegals and case managers typically handle the work. It requires familiarity with medical terminology and SSA evaluation criteria. Attorneys review completed chronologies and use them for hearing prep and brief writing.
How do treatment gaps affect a disability case?
Gaps raise questions about severity, and ALJs pay attention to them. SSA may infer that a claimant's condition improved if they stopped seeking treatment. The chronology should flag gaps and, where possible, document reasons: insurance lapses, provider unavailability, inability to afford care.
Moving Forward
A consistent medical chronology process reduces errors, improves hearing preparation, and creates better outcomes for claimants. The steps are straightforward: gather records, organize by date, extract key data, build the timeline, connect the output to brief writing and hearing strategy.
For firms handling significant case volume, the question becomes how to execute this process without creating staff bottlenecks or quality variation. Chronicle was built for Social Security disability practices. It focuses on SSA-facing operational workflows, including medical chronology management as part of hearing preparation.
Staff spend less time on data extraction and more time on case strategy.